Did you know that over 50% of people below the age of 50 have degenerative disc disease? Even more impressive, over 90% of people aged 60 years or older have this condition.
Degenerative disc disease (DDD) is a common condition affecting the cervical spine, or neck, that most everyone will have to deal with at one point during their life. The condition is characterized by a range of symptoms, including neck pain or arm complaints, resulting from an injured or damaged spinal disc.
Neural foraminal stenosis of the cervical spine affects millions of Americans each year, making it one of the most prevalent spinal conditions we treat. Understanding this condition, its causes, and treatment options is crucial for anyone experiencing neck pain or arm symptoms.
To learn more about cervical foraminal stenosis, keep reading.
What Is Foraminal Stenosis?
The bones of the neck are known as the cervical vertebrae. The discs between these bones act as shock absorbers and provide neck flexibility.
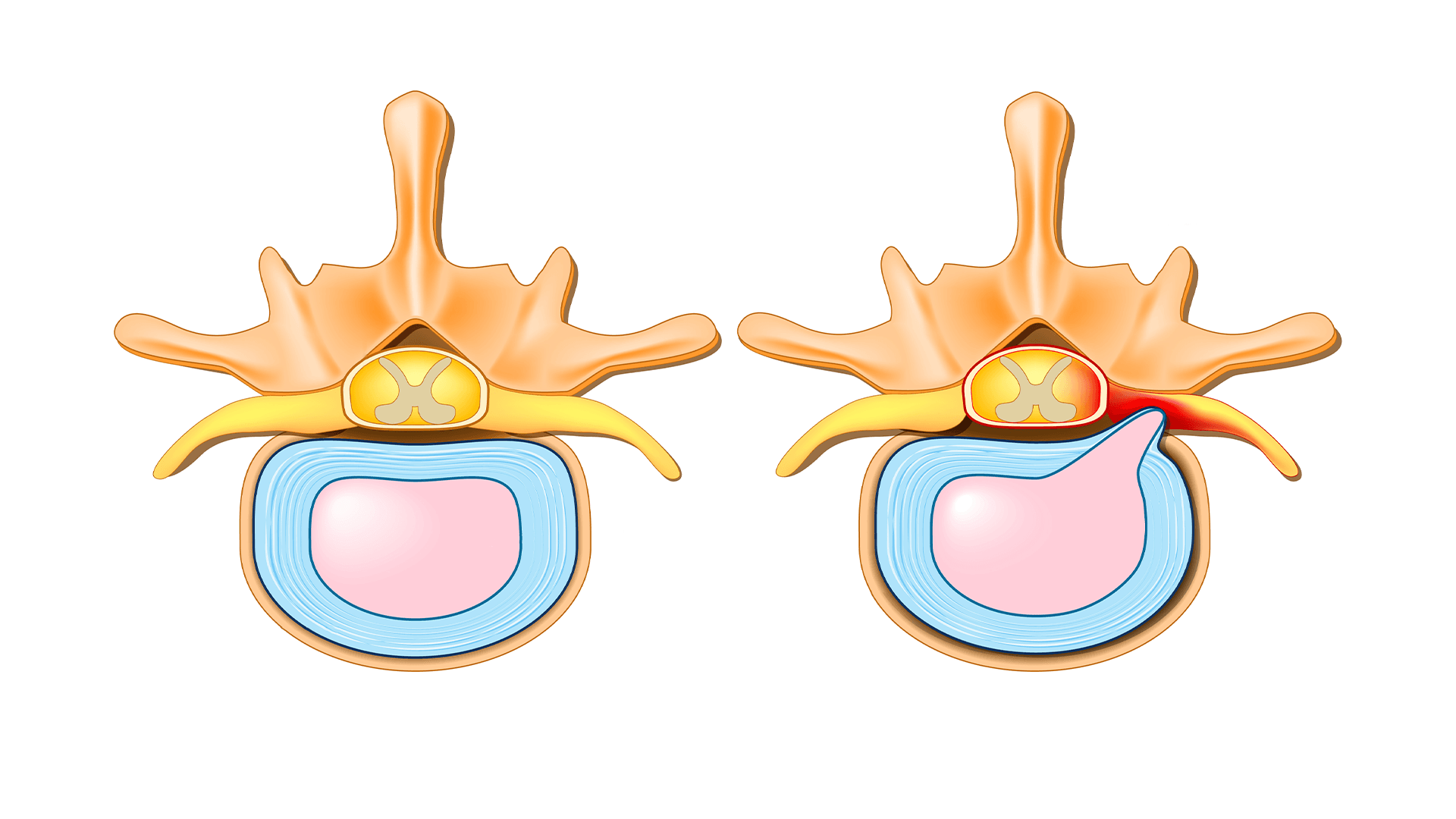
The spinal canal is the main channel within the vertebrae that contains the spinal cord and nerve roots. The foramen are the bony channels between the vertebrae where pairs of spinal nerves travel to our arms.
Neural foraminal stenosis of the cervical spine occurs when these critical nerve pathways become compressed or narrowed. The neural foramina in the cervical spine serve as the exit points for spinal nerves, and when narrowing occurs, it can significantly impact nerve function.
As we age, normal wear and tear leads to a damaged disc. This is aggravated by changes to the blood vessels that supply the disc, reducing the needed nourishment to keep the disc healthy. As the disc degenerates, bone spurs form that narrow the opening of the foramen, leading to pressure on the spinal nerve roots. This leads to cervical stenosis or narrowing, and when it involves the foramen, known as cervical foraminal stenosis.
Understanding cervical foraminal stenosis is essential for early recognition and treatment. This condition represents a narrowing of the neural foramina of the cervical spine, which can occur at single or multiple points along the spine.
Common causes or associated conditions of foraminal stenosis include:
- Herniated disc
- Bulging disc
- Bone spurs (osseous neural foraminal stenosis)
- Spondylolisthesis
- Degenerative neural foraminal stenosis
- Age-related disc degeneration
- Arthritis of the cervical spine
- Previous neck injuries or trauma
What Are the Symptoms of Cervical Foraminal Stenosis?
As a result of the degenerative changes, patients can develop a poor posture that leads to constant strain and stress of the neck muscles, resulting in chronic neck pain. This pain is typically localized to the neck or shoulder blades.
When the foraminal stenosis leads to pressure on the existing spinal nerves, the condition is commonly referred to as a “pinched nerve,” which can cause symptoms in the arm.
Symptoms of cervical neural foraminal stenosis can vary significantly depending on the location and severity of the narrowing. Patients with neuroforaminal stenosis of the cervical spine may experience a range of symptoms that can impact daily activities and quality of life.
Here are some symptoms that patients may begin experiencing due to the degenerative disc disease and cervical foraminal stenosis:
- Acute or chronic neck pain
- Pain that radiates into the arms
- Numbness and/or tingling in the arm
- Weakness in specific muscles of the arm
Additional symptoms of neural foraminal stenosis may include:
- Sharp, shooting pain that travels from the neck to the fingers
- Burning sensations in the affected arm
- Muscle spasms in the neck and shoulder region
- Sleep disturbances due to positional pain
When foraminal stenosis occurs higher in the neck, C3-C4 foraminal stenosis, for example, the pain is focused more heavily in the neck. When occurring at lower levels, C5-C6-C7, there is more involvement in the arms.
Different levels of involvement can create varying symptom patterns:
- Upper cervical levels (C3-C4, C4-C5): Symptoms tend to be more focused in the neck and upper shoulder region
- Mid-cervical levels (C5-C6): May involve shoulder, arm, and hand symptoms
- Lower cervical levels (C6-C7-T1): Often affect the arm and hand, potentially impacting grip strength.
The specific symptoms experienced can vary significantly between individuals, even with similar levels of involvement. Your healthcare provider can help determine which nerve roots may be affected based on your symptom pattern.
Bilateral neural foraminal stenosis symptoms occur when both sides are affected, leading to more widespread and severe symptoms affecting both arms.
Understanding Severity Levels
The radiographic severity of neuroforaminal stenosis of the cervical spine is typically classified as:
- Mild neural foraminal stenosis: Minimal narrowing with occasional symptoms
- Moderate neural foraminal stenosis: Noticeable narrowing with regular symptoms
- Severe neural foraminal stenosis: Significant narrowing causing persistent, debilitating symptoms
Severe bilateral neural foraminal stenosis represents the most challenging form, potentially affecting multiple nerve roots simultaneously. More important than the radiographic description is whether or not the stenosis is causing symptoms and their severity.
Is Cervical Foraminal Stenosis Serious?
Cervical foraminal stenosis can lead to nerve irritation or injury.
Patients with severe foraminal stenosis may experience more intense symptoms. Spinal nerves exiting lower in the neck, such as the C6 spinal nerve, act as both a sensory and a motor root to the arms.
This means that damage to these nerves could result in problems with both strength and sensation that can compromise a person’s ability to perform basic activities, such as lifting a coffee cup.
The severity of neural foraminal stenosis depends on several factors, including the degree of narrowing, the number of levels affected, and the resulting symptoms. Severe symptoms of neural foraminal stenosis can lead to permanent nerve damage if left untreated, making early intervention crucial.
The condition becomes particularly concerning when it involves:
- Progressive neurological deficits
- Significant functional impairment
What Happens if Foraminal Stenosis Is Left Untreated?
If left untreated, the condition could worsen and lead to permanent neurological injury.
We highly recommend that you consult a physician and seek medical advice as soon as possible if you suspect issues with arm sensation or strength.
Does neural foraminal stenosis go away on its own? Unfortunately, this degenerative condition leading to foraminal stenosis does not reverse. The structural changes that cause the narrowing generally worsen with age. If symptoms develop, early intervention may be crucial for preventing permanent nerve damage.
Potential complications of untreated neural foraminal stenosis include:
- Permanent nerve damage
- Chronic pain syndromes
- Progressive muscle weakness
- Loss of upper extremity sensation
- Disability affecting work and daily activities
How Is Foraminal Stenosis Diagnosed?
To diagnose foraminal stenosis, your physician will start with a detailed medical history. This will allow them to assess your pain, including its severity, location, and frequency.
A comprehensive neurological exam will be performed to determine if there are any neurological deficits, such as a loss of sensation or strength that is not pain-related.
Your physician may decide to get imaging of the spine. X-rays are the primary screening tool to ensure there is no significant deformity of the spine.
A CT scan provides excellent definition of the bones, while an MRI allows your physician to see the soft tissue structures, such as muscles, spinal nerves, and spinal cord. Contrast material is often not required to evaluate for cervical foraminal stenosis.
Modern diagnostic approaches for neuroforaminal stenosis of the cervical spine include:
- High-resolution MRI to evaluate soft tissue structures
- CT scans to evaluate the bones of the neck
- Dynamic imaging to assess positional changes
- Electromyography (EMG) and Nerve conduction studies to evaluate nerve function
The diagnostic process helps determine:
- The location of neural foraminal stenosis
- The degree of stenosis
- Single or multilevel involvement
What Is the Treatment for Foraminal Stenosis?
There are non-surgical and surgical treatments for foraminal stenosis.
Non-surgical Treatment Options
Non-surgical treatments include non-steroidal anti-inflammatory drugs, oral steroids, muscle relaxers, prescription pain medication, and physical therapy or chiropractic treatment. If these less-invasive maneuvers do not work, steroid injections may be considered.
Comprehensive non-surgical cervical neural foraminal stenosis treatment includes:
- Physical therapy focusing on neck stabilization and posture correction
- Cervical traction to decompress neural structures
- Targeted steroid injections (epidural or selective nerve root blocks)
- Dry needling and trigger point therapy
- Ergonomic modifications for work and daily activities
- Heat and cold therapy
- TENS units for pain management
- Activity modification and lifestyle changes
The treatment of neural foraminal stenosis conservatively depends on the severity and individual patient factors. Many patients with mild to moderate stenosis respond well to conservative management.
Surgical Treatment Options
When conservative treatments fail or severe neural foraminal stenosis symptoms persist, surgical intervention may be necessary. Surgery becomes the preferred option when:
- Conservative treatment fails after 6-12 weeks
- Progressive neurological deficits, such as muscle weakness, occur
- Severe pain significantly impacts quality of life and fails conservative care
Surgical options for severe neural foraminal stenosis treatment include:
- Anterior cervical discectomy and fusion (ACDF)
- Posterior cervical foraminotomy
- Cervical disc replacement
- Minimally invasive approaches
- Multi-level procedures for multilevel disease
The choice of surgical technique depends on the specific location, severity, and extent of the stenosis.
Prevention and Risk Factors
Understanding what causes neural foraminal stenosis can help with prevention strategies:
- Age-related disc degeneration
- Poor posture, especially forward head posture
- Repetitive neck motions
- Previous neck injuries
- Genetic predisposition
- Smoking, which reduces disc nutrition
Prevention strategies include:
- Maintaining proper posture
- Regular neck strengthening exercises
- Ergonomic workplace setup
- Avoiding prolonged static positions
- Smoking cessation
When to Seek Emergency Care
It’s important to contact your healthcare provider promptly if you experience:
- Worsening neurological symptoms
- Progressive weakness in your arms or hands
- New or worsening numbness that interferes with daily activities
- Symptoms that don’t respond to initial treatment
- Any concerns about changes in your condition
Your healthcare provider can best determine the urgency of your situation and recommend the most appropriate next steps based on your specific circumstances.
Treating Cervical Foraminal Stenosis and Other Neurological Conditions
Whether you suffer from cervical foraminal stenosis, degenerative disc disease, or a combination of issues, you should see a trained spinal specialist. The physicians at Neurosurgeons of New Jersey are specialists trained in the most advanced techniques to treat cervical or other spinal conditions.
Our team specializes in both conservative and surgical management of cervical foraminal stenosis. We understand that each patient’s experience with neural foraminal stenosis of the cervical spine is unique, requiring personalized treatment approaches.
If you’re having symptoms, you should call our team at Neurosurgeons of New Jersey and make an appointment.
Don’t let cervical foraminal stenosis symptoms compromise your life. Early diagnosis and appropriate treatment can significantly improve your quality of life and prevent progression to more severe conditions. Contact us today at 551-284-3265 to schedule a comprehensive evaluation and discuss your treatment options.

About Dr. Michael G. Kaiser
Dr. Michael G. Kaiser is a nationally recognized neurosurgeon in North Jersey and is a proud member of Neurosurgeons of New Jersey, practicing out of their Ridgewood office conveniently located on East Ridgewood Avenue. Dr. Kaiser specializes in complex and minimally invasive spine surgeries.
Please call today to schedule a consultation with me.
(551) 284-3265
Request a consultation with Dr. Kaiser