Understanding MMA Embolization: A Novel Treatment for cSDH
What is MMA Embolization?
Middle meningeal artery embolization MMA embolization, is a medical procedure used to treat cSDH (chronic subdural hematoma)
What is a cSDH?
Chronic subdural hematoma (cSDH) is the most prevalent neurosurgical condition among older adults. It is characterized by the collection of blood in the subdural space which causes compression of the brain resulting in neurological symptoms.
With the aging of the US population, researchers predict an ~80% increase cSDH prevalence between 2020 and 2040, with predicted annual incidence of over 200,000.
What are risk factors for cSDH?
cSDHs most commonly affect the elderly, with the mean age at diagnosis being late 70s. Head trauma – which can sometimes be mild, long term alcohol intake, and the use of blood thinners are the most common risk factors for cSDHs The use of anticoagulants increases the risk of cSDH by 42 times.
cSDH is different from acute subdural hematoma (SDH), in which a trauma causes sudden disruption of the dural vasculature, brisk bleeding and acute mass effect.
In contrast, cSDH is characterized by repetitive microbleeds and slow ongoing fluid leakage from inflammatory neovascular membranes. Not all acute SDH become chronic and not all cSDH start with trauma.
Pathophysiology of cSDH was previously believed to be venous in nature – specifically leakage from fragile bridging veins in the setting of tension due to brain atrophy. MMA embolization research has provided additional insight around the arterial contribution to this pathology. Specifically, the middle meningeal artery supplies overgrown inflammatory neovascular membranes with a propensity to repeatedly ooze.
How are cSDH diagnosed?
cSDH are typically diagnosed with CT scan or MRI of the brain.
It's time to get back
to doing what you love.
What are the symptoms of cSDH?
cSDH can cause a variety of symptoms including seizures, stroke-like symptoms which cause disability. A diagnosis of CSDH is a significant predictor of mortality, with an overall survival of ~ 4 years from diagnosis.
cSDH cause neurological disability and increase risk of mortality. Symptoms arise due to the displacement of the brain and include weakness, aphasia, visuospatial dysfunction and decreased level of consciousness.
They can also cause patients to present with non-specific symptoms such as falls, cognitive decline, confusion, Parkinsonism, fluctuating neurological deficits, and seizures.
SDH is associated with 40% risk of mortality. Mean survival for cSDH is ~ 4 years from the time of diagnosis.
What is the treatment for cSDH?
There are different treatment options available for the management of cSDH.
Prior to 2015, cSDH was classically managed with either observation for asymptomatic patients or surgical drainage for symptomatic patients.
Open surgical evacuation of the subdural blood is performed via small burr holes or a craniotomy in the skull. It is an invasive treatment associated with risks in patients who frequently have comorbidities. Despite drainage, cSDH can recur in up to 30% of patients.
How is MMA Emolization Done?
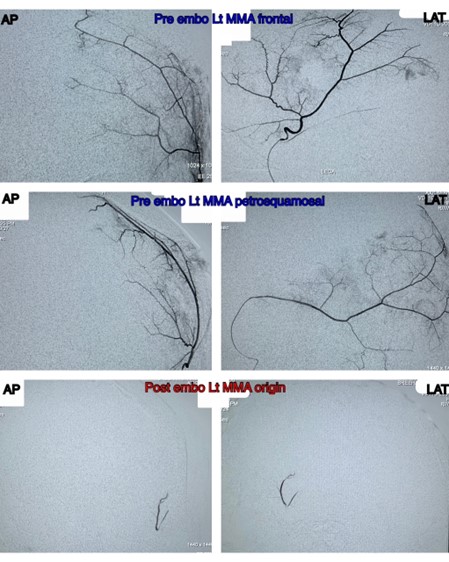
Middle meningeal artery (MMA) embolization is a minimally invasive procedure performed via trans-arterial catheters using angiography to guide the intervention.
Access is typically via a small puncture site in the right wrist called a trans radial approach. Radial access is safe and effective, and avoids complications associated with groin, or femoral artery access, and it minimizes the risk associated with aortic arch anatomy in older patients.
Embolic agents such as polyvinyl alcohol particles, are injected via microcatheters into the middle meningeal artery (MMA), the vessel which provides blood supply to the dura, until occlusion of the artery is demonstrated.
Other embolic agents include liquid embolics such as nBCA (N-butyl cyanoacrylate) and onyx. Occasionally small coils are used to close branches more proximally after the closure of the more distal arteries is performed.
The procedure is performed unilaterally (or bilaterally). Complications are uncommon, reported in fewer than 1-2% of cases. Risk is low because the intervention is performed via the external carotid artery and therefore catheterization of the intracranial or brain arteries is not needed. With good understanding of the anatomy to the dura and its potential collaterals to the brain and cranial nerves, major complications are exceedingly rare.
MMA embolization targets the vascular supply of the neomembranes implicated in cSDH pathophysiology and allows the body’s normal healing process of reabsorption of blood in the subdural space to unfold.
Embolization prevents re-accumulation of new blood, reducing recurrence rates from up to 30% to less than 5%. A recent manalysis comparing MMA embolization tp conservative care showed that 95% of patients treated with pure MMA embolization were able avoid surgery and had reduced volumes or cured cSDH on follow up brain imaging.
Embolization allows the body’s natural healing process of reabsorption of blood in the subdural space to unfold, and it prevents reaccumulation of new blood, reducing recurrence rates to less than 5%.
Recovery from MMA Embolization
Patients are typically discharged home one day after embolization with usual activities resumed within days. Adjunctive medical treatments to achieve normal blood pressure, and in patients without a history of diabetes, a short 2-4 week course of low dose steroids, can improve efficacy post embolization.
Follow up after MMA embolization involves a non-contrast head CT at 1 month and 6 months post treatment. The one month CT will demonstrate a reduction in the hematoma size and mass effect,. Complete normalization of findings including reabsorption of blood in the subdural space is typically seen by 6 months.
Benefits of MMA Embolization
We can now manage more than 90% of patients who previously would have met criteria for open surgery with pure embolization, reserving transcranial surgery for the most symptomatic patients. MMA embolization is now the standard of care for subacute and cSDH at major neurointerventional centers. It is used as an adjunctive treatment in combination with drainage in some cases and as a stand‐alone treatment for patients with mild symptoms.
MMA embolization is a safe and effective option to treat cSDH, both as adjunct therapy to prevent recurrence in surgically evacuated cSDH and as a stand‐alone procedure to treat both asymptomatic and symptomatic cSDH.Nuanced decision algorithms for patient selection are still being defined with ongoing research. Current trials underway with expected completion in 2024 include STEM (The SQUID Trial for the Embolization of the Middle Meningeal Artery for Treatment of Chronic Subdural Hematoma),https://www.ahajournals.org/doi/10.1161/SVIN.122.000490
EMBOLISE (Embolization of the Middle Meningeal Artery With ONYX Liquid Embolic System for Subacute and Chronic Subdural Hematoma), and MEMBRANE (Middle Meningeal Artery Embolization for the Treatment of Subdural Hematomas With TRUFILL n‐BCA).
REFERENCES
Increases in Subdural Hematoma with an Aging Population—the Future of American Cerebrovascular Disease
A portion of the results were presented at the Congress of Neurological Surgeons 2019 Annual Meeting as a digital poster from October 20, 2019–October 23, 2019 in San Francisco, California.
Author links open overlay panelSean N. Neifert, Emily K. Chaman, Trevor Hardigan, Travis R. Ladner, Rui Feng, John M. Caridi, Christopher P. Kellner, Eric Karl Oermann
Middle Meningeal Artery Embolization to Treat Chronic Subdural Hematoma
Robert F. Rudy, Joshua S. Catapano, Ashutosh P. Jadhav, Felipe C. Albuquerque and Andrew F. Ducruet
Originally published26 Dec 2022https://doi.org/10.1161/SVIN.122.000490Stroke: Vascular and Interventional Neurology

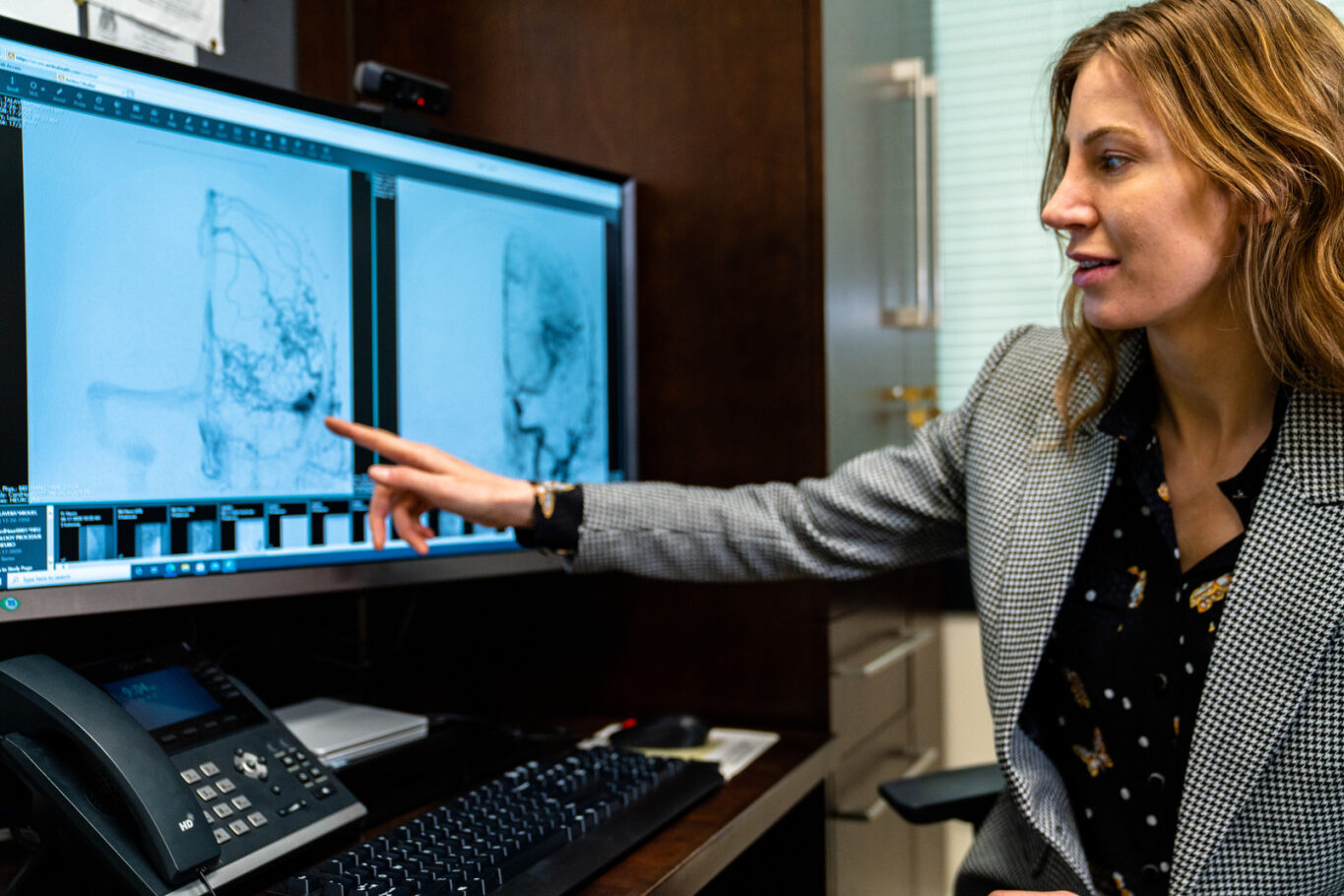
About Dr. Bree Chancellor
Dr. Chancellor is a Neurointerventionalist specializing in the endovascular treatment of vascular disorders of the brain and spine including aneurysms, acute stroke, arteriovenous malformations and fistulas, carotid and intracranial atherosclerotic disease, spinal and facial vascular lesions, spinal fractures, and brain tumors. She is facile in the latest proven minimally-invasive neurointerventional techniques including flow diversion, transradial angiography, subdural hemorrhage embolization and transvenous stenting. Dr. Chancellor accepts a range of health insurance and sees patients in Paterson, NJ and Ridgewood, NJ.