Minimally Invasive Lumbar Fusion Overview
Minimally invasive lumbar fusion is a range of surgical techniques and technology. This allows doctors to perform spinal fusion surgery with smaller incisions resulting in much faster recovery times.
it is one of the biggest advancements in spine surgery in the last 25 years. It is important to know the benefits of minimally invasive lumbar fusion and why it is performed.
What is lumbar fusion surgery?
Lumbar fusion is a surgical procedure that is usually performed to treat leg pain from compressed spinal nerves. It can also help treat back pain from degenerative disc disease or degenerated spinal joints. Sometimes spinal nerve compression can cause leg or foot weakness or numbness, and surgery can help with these symptoms as well.
Lumbar spinal fusion usually involves the removal of tissue (bone, ligament and/or disc material) that is pushing on spinal nerves. Then, over time, two spinal vertebrae that used to be connected by a joint grow together to become a single bone. This second part of this process is known as the “fusion.”
The benefits of spinal fusion include improvement in nerve-related symptoms. It also helps to improve symptoms that can result from abnormal, excessive movement across the spinal joint. These movements cause a wearing down of cartilage over time so that it no longer provides “cushioning” with normal joint movement.
What conditions does lumbar fusion treat?
Minimally invasive lumbar fusion surgery can be used to treat a number of conditions.
The most common conditions treated with lumbar spinal surgery are:
- Spondylolisthesis- a condition where the spinal vertebrae are not lined up correctly
- Pars Defect or spondylolysis
- Severe degenerative disc disease
- Spinal stenosis/lumbar stenosis
- Herniated discs-usually if the same disc has herniated more than once
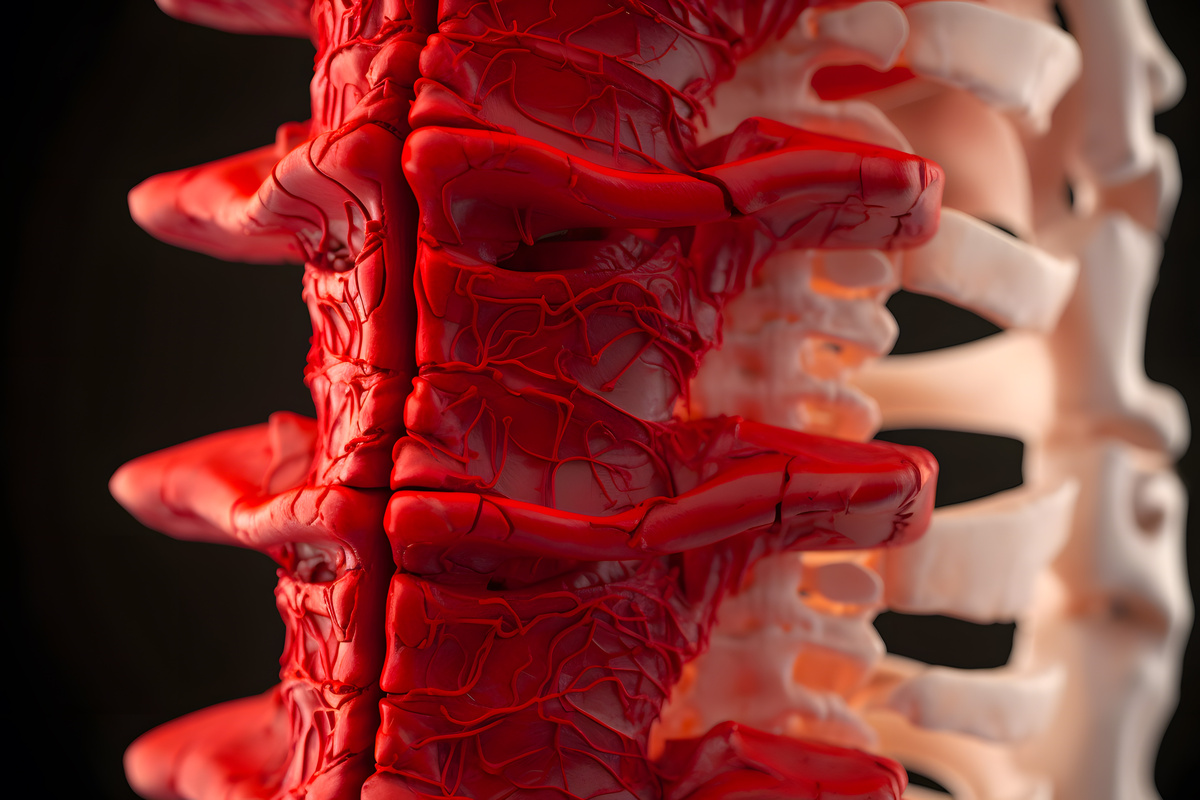
What is the lumbar spine?
To understand how a lumbar fusion is performed, it is useful to understand a little spinal anatomy. The “lumbar” part of the spine is commonly referred to as the “lower back”. It is the part of your spine that connects your rib cage to your hips and pelvis.
The lumbar spine has vertebrae, or bones, connected to each other by an intervertebral disc at the front. At the back, there are two joints known as the facet joints.
Most people have a spinal cord that ends near the beginning of the lumbar spine. It then transitions into nerve roots. Nerve roots run down the lumbar spine, they exit the spine at intervals between the vertebrae.
The lumbar spine’s nerve roots transition into two sets of nerves. The first set goes to the legs and feet. The second set controls urination, bowel movement and sexual function. All the important major blood vessels are in front of the spine behind the organs in the abdomen.
The lumbar spine is essential for walking on two feet. It also protects the important nerves that control the lower body, all while allowing a good amount of movement and flexibility.
How is Spinal Fusion Performed?
There are a variety of techniques used to perform lumbar spinal fusion. This is in part because the growing together of the vertebrae or “fusion” can occur anywhere that the bones are in close proximity.
Historically, mostly posterior spinal fusion was performed. This involved removing all the muscle attachments off of the posterior part of the vertebrae and laying down bone graft material directly onto the posterior surface of the spine. This is called an “on-lay fusion.” Patients would stay on bedrest for weeks to allow bone growth to get a head start before putting pressure on it.
Then spinal instrumentation was invented. First came bone screws (pedicle screws), and a way to connect them using rods. This technique was a major improvement. It offers instantaneous stabilization of the bone during the healing process of fusion, which allows patients to move right away.
It's time to get back to doing what you love.
The next big advancement was the utilization of blocks of bone. Later on came metal and carbon fiber, which could be placed in between the vertebral bodies after removal of the intervertebral disc, in the space that the disc used to occupy, along with other kinds of bone graft material.
This kind of fusion is called an “interbody fusion” and can be performed from the front of the abdomen in what’s called an anterior lumbar interbody fusion.
When performed from the side it’s called a transpsoas interbody fusion, or from the back in what’s called a transforaminal lumbar interbody fusion.
Initially interbody was thought to be a good idea because it would provide additional stability and additional surface area for fusion, thereby helping the healing process.
What is minimally invasive lumbar spinal fusion surgery?
Eventually, it was realized that interbody fusions alone were sufficient and on-lay fusion were not necessary. Large incisions and extensive stripping of muscle from the bone were no longer required for interbody fusions. In most cases, the incisions only need to be a little bigger than whatever implant is going through it.
This is possible because you can stretch muscle and most other soft tissue without injuring it or disconnecting it. It can also be dilated with tubes made from metal or plastic that slide over each other, making the opening larger. Surgeons can then use the final tube to operate through.
Even the final tube or tubular retractor, as it’s called, doesn’t even need to be very big! When the surgery is done, and the retractor is removed, the muscle slides back into place with very little injury.
This concept of muscle dilation was first applied to interbody fusions performed via a posterior approach, and this is most popular way to perform a minimally invasive lumbar fusion today. The technical name for this procedure is a minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF).
Through two half-inch incisions in the back, surgeons perform a lumbar fusion that involves nerve root decompression (laminectomy), placement of cage and bone graft material (interbody fusion), and placement of bone screws (pedicle screw fixation).
More recently, the same concept and techniques have been applied to anterior spinal fusion performed either through a lateral/flank incision (transpsoas interbody fusion) or an anterior/abdominal incision (anterior lumbar interbody fusion).
The advantage to these anterior/lateral approaches is the ability to put in bigger cages than with a posterior approach. The disadvantage is that direct nerve decompression and pedicle screw placement require additional incisions when an anterior approach is chosen.
What are the benefits of minimally invasive lumbar fusion?
There is less muscle damage after surgery, and this enables you to increase your activity level more rapidly than after traditional spine fusion. Multiple studies have demonstrated these benefits and have also shown at least as good long-term outcomes.
What is the recovery after Minimally Invasive Lumbar Fusion like?
Every patient heals differently, but most patients go home within 24-36 hours after minimally invasive lumbar fusion and then gradually get back to normal activities. Your doctor may have you start a walking program to help you regain your mobility and overall endurance..
For most patients the first two weeks are the most difficult. Patients are limited to being around the house and require prescription pain medicine to function. After a few weeks of healing, most are feeling well enough to return to everyday activities.
Your doctor may allow you to return to work if your job does not require heavy manual labor or lifting. After 6-12 weeks, most people can begin low impact exercise. At some point within this time frame, physical therapy is usually beneficial.
You may have to avoid high intensity athletics or very physical work until adequate healing of the fusion has taken place. This can potentially require several months.
Risks of Minimally Invasive Lumbar Fusion
Every surgical procedure carries with it some risks, and minimally invasive lumbar fusion is no different. Typical risks of the procedure include:
- Spinal fluid leak
- Infection
- Hematoma
- Nerve irritation or injury
- Instrumentation problem
- Failure of bones to heal over time, also known as a “non-union” or “pseudoarthrosis”
The risks from minimally invasive lumbar fusion are no different when compared to an open spinal surgery.
Surgery can be a scary prospect for many people, especially when they hear about the risks. , It is important to keep in mind that the vast majority of patients recover from minimally lumbar fusion without complications.
Is Minimally Invasive Lumbar Fusion Right for Me?
It is natural to be concerned about any surgery, and many patients are worried about facing lost time at work or with family.
Most healthy and active people who undergo minimally invasive lumbar fusion surgery can get back to work and family within 2-4 weeks. Overall, the results from these surgeries are excellent. Finding a good surgeon is the most important thing. They should have a lot of experience performing these surgeries and know which patients are suitable candidates.

About Dr. Alfred T. Ogden
Dr. Alfred T. Ogden is an accomplished neurosurgeon in North Jersey and is a proud member of Neurosurgeons of New Jersey, practicing out of their Ridgewood office conveniently located on East Ridgewood Avenue. Dr. Ogden is internationally recognized as a leader in minimally invasive spine surgery.